 In the past few months, Adventist HealthCare Shady Grove Medical Center in Rockville has hired nearly 50 additional nurses and prepared a second intensive care unit for incoming COVID-19 patients.
In the past few months, Adventist HealthCare Shady Grove Medical Center in Rockville has hired nearly 50 additional nurses and prepared a second intensive care unit for incoming COVID-19 patients.
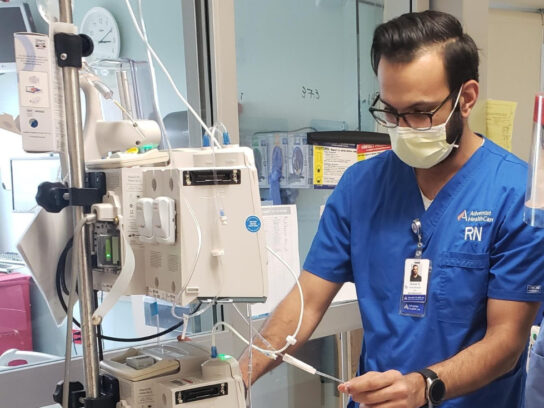
And while Intensive Care Unit Nurse Manager Nimeet Kapoor believes his crew is ready and well equipped for the patients who keep coming, he knows he must continue preparing for a possible new surge in cases.
“I am hoping we are at the peak right now,” he said.
Along with seeing patients, Kapoor spends his day recruiting staff, purchasing masks, ventilators and other equipment making sure there are empty beds.
The Rockville resident estimated that a little more than half of the patients currently in ICU are COVID-19 patients, although COVID-19 patients are spread throughout the hospital and not just in critical care sections.
Those that he sees in the ICU are quite ill, often on ventilators.
“We are seeing sicker patients for sure,” Kapoor said. “A lot of patients coming in don’t have underlying” medical problems like diabetes and hypertension.
“The majority, they are pretty healthy otherwise,” before getting the novel coronavirus, he said.
Those in ICU, “They are truly sick. Many of them are on ventilators and end up staying on ventilators for a long period of time.”
Within the past two weeks, there has been a surge of new cases but that seems to have leveled off, Kapoor said, noting that he is hopeful a new surge is not on the horizon.
He considers his hospital “fortunate to have a bit of a time line before the surge,” and was able to gather extra equipment and staff.
“I don’t think anybody is ready for it. I think everybody is a little overwhelmed by it.”
Emotionally, it has been extremely difficult for everyone, especially the patients who must face their treatment and medical issues by themselves. The hospital closed its doors to visitors so as not to spread the disease.
Normally, “we like when someone is with them during these times,” Kapoor said of ICU patients who often are sedated and on ventilators.
The staff tries its best to provide support. At least once a day, someone telephones the patient’s family and updates them on their loved one’s condition.
“I’ve seen one of my nurses just go in and just hold their hand, just to give them that comfort,” Kapoor said. “The human factor, we don’t want to lose that.”
Also, the hospital’s chaplains have continued making their rounds.
It is not just the patients struggling with their emotions. So, too, is the staff.
“It is definitely challenging at times to keep your spirits up,” he said. “The stress levels are high everywhere, not just the ICU.”
He likes to remind his staff that everyone is in this together.
“We will be together. We will stick together, and we will come out of this together,” he tells them.
“Our community has been great, giving us lunches, dinners and donating supplies,” Kapoor said. All the little things people do are “very helpful, very uplifting.”
But truly the best times are when a patient leaves the ICU. “It is very uplifting for us as health care providers,” he said.
When the nurses end their shift, they go their separate ways. “Some people are staying in hotels. Some people are staying in their basements, and some people aren’t doing anything different, just coming out of their scrubs,” he said.
Kapoor changes out of his work clothes at the hospital and immediately takes a shower before seeing his significant other and dogs.
Kapoor, who previously worked at the University of Maryland Medical Center, would love everyone to stay at home as much as possible and always wear a mask when venturing out. And keeping washing their hands.
Unless someone has major symptoms, he does not believe they need to be tested for COVID-19.
“In my personal opinion, I don’t think a test is important if you are healthy otherwise,” he said.
For those with minor symptoms, Kapoor suggested they take their temperature regularly.
He is concerned that people needing medical treatment not related to the virus are staying away from the hospital and believes they are “absolutely” scared to enter the emergency room.
Hopefully, they are receiving medical treatment elsewhere, he said.
He wants everyone to know that his hospital is prepared to take care of all patients.
Recently, the hospital brought on 40 to 50 extra nurses.
Prior to COVID-19, there were nine to 10 nurses on each shift in the ICU. There are 20 per shift now, he said. The new nurses are agency or traveling nurses and have temporary contracts.


Comments are closed.